HIGH PRECISION BIOMETRY
DR. REZAUL MURSHED
M.B.B.S(D.M.C)D.O
CONSULTANT
AHMAD MEDICAL CENTER
E mail: amc@bol-online.com
INTRODUCTION
APART FROM THE EXCELLENT SURGICAL TECHNIQUES PRE-OPERATTIVE BIOMETRY IS VERY IMPORTANT IN PREVENTING REFRACTIVE SURPRISES POSTOPERTIVELY.
SIR HAROLD RIDLEY
DID HIS FIRST IOL SURGERY THE POST-OPERATIVE REFRACTION WAS +24DS/6.00*30
PERFECTION NEEDS
CONSISTENCY & ACCURACY OF IOL POWER CALCULATIONS
ACCURATE MEASUREMENT AL & KERATOMETRY
WHICH FORMULA WE SHOULD FOLLOW
ALL MEASUREMENT
BY ULTRASOND
Applanation (Contact) A-Scan
Immersion A-Scan (To get accurate AL/like IOL master)
Immersion A/B Scan
BY SHORT WAVE LENGTH LIGHT OPTICAL COHERENCE BIOMETRY
IOL Master, best but (Disadvantage axial opacities &Very expensive too!)
KERATOMETRY
MANUAL KERATOMETRY(CHEAP)
AUTOMATIC KERATOMETRY(COSTLY)
SECOND MOST IMPORTANT AFTER AL
KERATOMETRY
1 D error in Keratometric reading would lead 0.9 D error in the calculation of IOL power.
Gonioscopy & Tonometry before keratometry should be avoided as it distorts the mires.
Putting artificial tear before Keratometry
Neutralise (+) mire first than (-) mire
Correct eye piece setting before Keratometry
Diopteric power between 40D> to <50D
Frequently check calibration of the Keratometer
FORMULA
BEFORE 1975 IOL=18+(1.25XRefrcation)
Error exceeding 1D occurred over 50%> some errors large as 9D refraction surprise. Now a number of formulas for IOL calculations Published since 1980.
Based on accurate measurement of
Corneal power
Axial length
Now modern formulas include
Corneal power
Axial length
Estimated lens position
Anterior Chamber (ELP) depth
WHICH FORMULA TO CHOOSE
Every Surgeon Should Personalize his
A-Constant,SF,aO,a1&a 2
SRK II works well AL between 22 to 24.5mm
SRK T & Hoffer Q works well AL < 21mm
Holladay 2 very good in high myopia
Haigis for all axial lengths
PERSONALIZATION/OPTIMIZING (To make perfect)
The concept of personalizing a formula based on a surgeon's past experience and data was introduced by Retzlaff using the A constant to refine the formula.
Holladay personalize his backsolving SF
Hoffer q backsolved his personalized ACD
Haigis personalized his a0(A- Con),a1(ACD),a2(AL)
Optimizing constants a0,a1,a2 for HAIGIS (hill@doctor-hill.com/w.haigis@augenklinik.uni-wuerzburg )
If you send the following data to Dr.Hill or Dr.Haigis he will send your own a0,a1,a2 at least 50 to 100 patients.
IOL Manufacturer ALCON, Model SA60AT,ACD 5.20
Pt.ID K 1 K 2 ACD AL SPH CYL IOL 1 42.25 43 3.58 24 +.25 00 19 100
FORMULAS
First IOL power formula was published by FYODOROV(1967)
FIRST GENERATION
SRK (SANDERS RETZLAFF-KRAFF)
SECOND GENERATION
SRK II, BINKHORST(1988)
THIRD GENERATION
SRK-T, HOLLADAY 1 and HOFFER Q
FOURTH GENERATION
HOLLADY 2 (1996) ,HAIGIS (LATEST)
SEVERAL VALUES NEEDED IN IOL POWER
Accurate Corneal power
Actual axial length
Accurate prediction of estimated lens position(1/2 mm shift may cause dramatic change on final vision)
A good understanding of various IOL power formulas is also required.
It is very important to discuss with patients their postoperative refractive expectations.
MEASURING AL IS THE KEY FOR IOL CALCULATIONS
1-mm error in measurement of axial length will give you 3 D error post operative refraction.
Between two eyes it varies .1mm normally but should not exceed >.3mm
Majority of AL 22mm-24.5mm(18D-22D) 72%
BASED ON AL
HOFFER(USA) |
|
KENNETH J |
FORMULA |
% |
AXIAL LENGTH |
SRK II |
72% |
22mm-24.5mm |
Holladay I |
15% |
24.5mm-26mm |
SRK/T |
05% |
26mm> |
Hoffer Q |
08% |
<22mm |
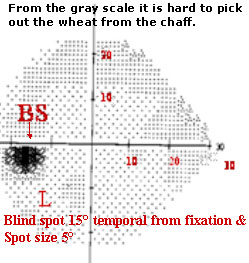
ROLE OF A-SCAN SPIKE
ACCEPT ONLY A STEEPLY RISING RETINAL SPIKE
ACCEPT A STRONG SCLERAL SPIKE ABOUT 1.5mm to 2mm POSTERIOR TO RETINAL SPIKE
ACCEPT A SERIES OF ORBITAL FAT SPIKES IN DESCENDING AMPLITUDE
SPIKES OF RxP
FORMULAS
SRK/T&SRKII FORMULA - USES A-CONSTANT
HOLLADAY 1 FORMULA -USES SURGEON FACTOR(SF=118.4x.5663 - 65.6=1.45) Alcon SA60AT
HOLLADAY 2 FORMULA USES ACD
HOFFER Q USES ACD(5.2 in Alcon's SA60AT)
Haigis uses three constants a0,a1&a2
a0=1.513,a1=.4,a2=.1(Alcon SA60AT)
A-CONSTANT
A Constant includes multiple variables that include the
Implant manufacturer
Implant style
Surgeon's technique
Implant placement within the eye
measuring equipment
H.John Shammas Page 18
New Terminology ELP & ALP
ELP effective lens position by Holladay or ALP actual lens position by FDA
ELP=aACD+ SF distance between the corneal vertex and IOL's optical center
aACD =anatomical AC distance between corneal vertex & iris
SF (Surgeon factor) distance between iris plane & IOL's optical center
PSEUDOPHAKIC EYE
WHY HAGIS IS LATEST FOR ALL LENGTH OF EYES !
Effective lens position is d d=a0+(a1*ACD)+(a2*AL)
Haigis uses three constant in his formula
a0=tied to A constant =118.4x.62467- 72.434=1.513(ALCON SA60AT)
a1=.4 constant is tied to the measured anterior chamber depth.
a 2=.1constant is tied to the measured axial length
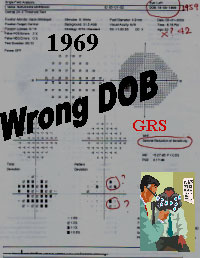
PROBLEMS OF IOL CALCULATION
Uses of an older, outdated IOL formula
Incorrect measurement of AXIAL LENGTH
Incorrect keratometry readings
Mistake in entering IOL calculation program
Incorrect labeling of IOL by manufacturer
Mix-up with an IOL for another patient
ULTRASOUND
Ultrasound machine does not measure the AL or distance directly.
Instead it measures the time (T) it takes the sound to traverse the eye and converts it to a linear value using the velocity formula D=VxT (24mm=1532m/sec.X.01566)
So, appropriate sound velocity settings is essential for obtaining accurate AL
Velocity of sound
1,532m/sec A-Scan Biometry (CALF)
Some US machine use single sound velocity 1555,1553,1550,or 1548m/s for phakic eyes.
Above values does not work well for all AL lengths.
For 29mm eye 1550m/s & 20mm 1560m/s
This is the reason why Long & Short eyes tend to be less accurate, in spite of very best technique.
Corrected axial length factor (CALF, +.32)
To avoid this error in AL Holladay took all eyes at a velocity of 1532m/s aphakic eye as bag of water
US machine sets at 1532m/s to measure the AL
Here true AL length is obtained by adding (.04mm cornea+.28mm Lens)= +.32mm(CALF) to the displayed axial length.(22+.32=22.32)
This new(22.32mm) number is then used for IOL calculation.
Velocity conversion equation
Cornea= T cX(1- 1532/1541)=.55x.066423=.04mm
Lens= TLX(1- 1532/1541)=4.21x.066423=.28mm
So, CLAF=.04mm+.28mm=+.32mm
ERRONEOUSLY SHORT EYE
CORNEAL COMPRESSION (CONTCACT )
SOUND VELOCITY TOO SLOW
RETINAL GATE IN VITREOUS CAVITY
GAIN SET TOO HIGH
LENS MEASURED TO THIN
MACULAR THICKNENING/R.DETACHMENT
MISALIGNMENT OF THE SOUND BEAM
ERRONEOUSLY LONG EYE
AIR BUBBLE IN FLUID BATH (IMMERSION)
FLUID BIRDGE(CONTACT METHOD)
SOUND VELOCITY TOO FAST
GAIN SET TOO LOW
LENS MEASURED TOO THICK
POSTERIOR STAPHYLOMA
MISALIGNMENT OF SOUND BEAM
BIOMETRY IN CHILD
| NORMAL AXIAL LENGTH VALUES |
| Age |
AL mm |
New born |
17.02 |
10-45 days |
17.22 |
46-75 days |
18.77 |
76-120 days |
19.43 |
5-9 months |
20.09 |
10-18 months |
20.14 |
19-36 months |
22.01 |
4-5yrs |
22.78 |
6-7yrs |
22.56 |
8-10yrs |
23.12 |
CURRENT APPROACH
UNDER CORRECTION
- 20% ............. 1-2yrs
- 15% ............. 2-4yrs
- 10% ............. 4-8yrs
- After 10yrs PLANO
Ashok Garg Jaypee
1yr. Old if IOL 28D Under correct by 20% 22.5 D To be implanted with +5 Spec
| Age |
3 |
4 |
5 |
6 |
7 |
8 |
10 |
13 |
| Goal |
+5 |
+4 |
+3 |
+2.25 |
+1.5 |
+1.0 |
+.50 |
Plano |
PREVENTION OF COMMON ERRORS
Ensure well trained, experienced person performing biometry and keratometry on a daily basis.
Check calibration of A-sacn & Keratometry on a daily basis.
Perform biometry in both eyes, for comparison
Between the two eyes there cannot be more than .3mm difference in AL (Unless anisometropia)
Use third generation Holladay, Hoffer Q, SRK T, Haigis
Immersion A-scan/IOL master, for AL
Use CALF for AL measurement
PREVENTION OF COMMON ERRORS
After calculating the scan, double check numbers to ensure the proper numbers were inserted into the program
Patient's pre cataract refraction
Good biometry machine (Latest formula)
Lens should be in the operating room before sedation/anesthesia
ADVANCEMENT
AROUND 1990,WITH THE FORMULAS AVAILABLE AT THAT TIME,BEING WITHIN ± 1.00 D OF TARGET REFRACTION WAS CONSIDERED A HIGH STANDARD
TODAY BY PAYING CAREFUL ATTENTION TO DETAIL, IT IS POSSIBLE TO BE WITHIN ± 0.50 D IN 95% OF SURGERIES OR BETTER.
RxP
S-15
RxP

FEW TIPS
LONG H/O EMMETROPIA NEED 18-22 D
LONG TIME MYOPE NEED <18 D
HYPEROPE NEED >22 D
ANY CONFUSION REPEAT BEFORE SURGERY
IMMERSION TECHNIQUE IS THE CHOICE
ERROR WITH CONTACT METHOD
CORNEAL COMPRESSION
A FLUID MENISCUS BETWEEN PROBE AND CORNEA
MISALIGNMENT OF SOUND BEAM
ADVANTAGE OF IMMERSION
OBVIOUS ADVANTAGE is CORNEA CANNOT BE COMPRESSED
PRAGER SHELL & PROBE WORKS AS A SINGLE UNIT
THUS GOOD ALIGNMENT OF SOUND BEAM ALONG VISUAL AXIS
WISE TO MEASURE AL IN DIFFICULT CASES STRABISMUS,NYSTAGMUS, BLEPHAROSPASM, POSTERIOR STAPHYLOMA
IMMERSION TECHNIQUE(IT)
OSSINIG shown IT more accurate than standard applanation & equal to IOL master over last 15yrs.
Argument against IT are that time-consuming, expensive, messy and requires the patient to be supine.
But new shell immersion technique are becoming popular for giving accurate IOL power.
Types of Immersion Technique
The Kohn Shell
Hansen Shell
Prager Shell
HANSEN SHELL
TYPES OF IMMERSION SHELL
KOHN SHELL BSS
HANSEN WITH METHYL CELLULOSE 1%
THE US PROBE IS IMMERSED IN SOLUTION , KEEPING IT 5 TO 10 mm FROM CORNEA
PRAGER SHELL

Prager Shell
Developed by Thomas C.Prager, Phd 1982
The accuracy of Prager Shell immersion biometry = optical biometry (IOL master)
Immersion US not limited by media density
Accurate insertion of US probe
Easy side tube connection
Clear shell for improved visibility
Uesd by 3,000 opthalmologist worldwide
CONCLUSION
VERIFYING MEASUREMENTS WHEN NECESSARY
RELY EITHER IMMERSION US OR OPTICAL COHERENCE BIOMETRY
OPTIMIZING LENS CONSTANTS
GOOD CAPSULORHEXIS SLIGHTLY SMALLER THAN IOL OPTIC
PC RUPTURE WITH VITREOUS LOSS/SULCUS FIXATION
 PC Ruptures
PC Ruptures 
Target IOL 22 D
IOL in Sulcus  Approx 0.5 to 0.75mm more anteriorly
Approx 0.5 to 0.75mm more anteriorly
the highlighted IOL calculation power will be the power to be implanted. Am I right?
Yes, that is the calculated power
I am asking this question as ultrasound probe remains 5-10mm from the cornea. I am facing some problem to keep BBS in the shell. Very often it leaks through the limbus, then I have to push BSS again from the syringe.
I do not have this problem. I apply slight pressure on the eye with the patient looking straight forward and there is no leakage. It will take about five patients for you to become skilled with the procedure.
I will be glad if you have any comment on Hansen shell.
The Hansen shell is an open cylinder and you have to add Goniosol. It is difficult to use because you need to be at a certain distance from the cornea for the RxP to acquire the signal and you also must be perpendicular to the fovea. The Prager shell does this for you and is a one-handed procedure. Using the Hansen shell is a two-handed procedure that takes a long time to learn
sincerely,
tom prager PhD
NEXT DISCUSSION
IOL POWER CALCULATIONS IN POST LASIK PATIENTS
IOL POWER CALCULATION AFTER KERATOPLASTY
IOL POWER WITH CORNEAL DYSTROPHY
IOL POWER CALCULATIONS IN CENTRAL CORNEAL SCAR/PTERYGIUM/ASTEROID HYALOSIS/CORNEAL LACERATION
IOL POWER CALCULATIONS WITH SILICON OIL
IOL POWER CALCULATIONS AFTER MACULAR HOLE SURGERY
IOL POWER CALCULATIONS WITH EXTREME MYOPIA 27mm>
COMMENT
ANY CONSTRUCTITIVE COMMENT IS MOST WELCOME. I WILL BE MOST HAPPY IF ANYBODY LEARNS A SINGLE WORD FROM THIS CD & MORE HAPPY IF HE/SHE TRANSMITS THIS TO HIS/HER FELLOW.
FURTHER READINGS
ULTRASOUND of the EYE and ORBIT SANDRA FRAZIER BYRNE & RONALDL.GREEN SECOND EDITION 2002
INTRAOCULAR LENS POWER CALCULATIONS H.JOHN SHAMMAS 2004
MASTERING THE TECHNIQUES OF IOL POWER CALCLATIONNS Ashok Garg,Jaior E Hoyos, Dimitrii Dementiev First edition 2005
THANK YOU ALL